1. To address the doctor shortages particularly in rural areas, a growing number of states are easing licensing for foreign-trained physicians. The changes involve medical residencies, which traditionally required foreign-trained doctors to repeat once in the U.S. before obtaining a full medical license. However, since 2023, nine states have eliminated this requirement for doctors with international training. Around 26% of practicing doctors in the U.S. were born overseas and need federal visas to live in the country and state licenses to practice medicine. Advocates argue that qualified doctors should not have to complete a second residency, but opponents question patient safety and the efficacy of easing doctor shortages.
2. Johns Hopkins pediatric faculty members and Baltimore-based community organizations are responding to the critical needs of young Latinx immigrants, who are often vulnerable to human trafficking. Support programs such as Steps to Success, initiated by Asylee Women Enterprise (AWE) and Johns Hopkins’ HEAL Refugee Health & Asylum Collaborative, provide therapy, peer support, and academic, employment, and skill-building opportunities. Meanwhile, Johns Hopkins’ Center for Salud/Health and Opportunities for Latinos (Centro SOL) focuses on the well-being of Baltimore’s growing Latinx community. Moreover, Dr. Keith Martin, a pediatrician at Johns Hopkins, is studying the barriers and health disparities faced by Latinx children in immigrant families to provide better trauma-informed care.
3. With President Trump’s pledge to crack down on immigration, health professionals warn of a potential healthcare crisis, especially among immigrant communities. Immigrants play a significant role in the U.S. health system, with many occupying critical lower-level positions such as nurses’ aides and community health workers. Enforced immigration could exacerbate the already critical health worker shortages in the U.S, particularly in rural areas. As of 2023, there is a projected shortage of more than 78,000 registered nurses nationwide. It is feared that fear of deportation could inhibit immigrants and their families from seeking necessary medical help.
News Article Summary:
1. Immigrants in the US are advised to carry original documents or copies that establish their identity and status in the country. The type of documents recommended varies based on the individual’s immigration status, i.e., current immigration status, pending status, in removal proceedings, or undocumented. For example, “Lawful Permanent Resident” proof or “Employment Authorization Card” should be carried by immigrants with a current immigration status. However, immigrants whose status is pending or who are in removal proceedings are advised to carry documents like copies of USCIS receipts or Notices of Hearing. Undocumented immigrants are advised against carrying false documents or their national passport, as these may be used against them in court.
2. A group of medical students at UC Davis was awarded first place at the Latino Medical Student Association (LMSA) 2023 National Conference for creating a poster describing a free health program for immigrants. The program provides physical exams for immigrants applying for green cards, easing the burden of expensive private practice doctors. Now dubbed the Immigration Medical Exam (IME) clinic, the program operates under the supervision of a community physician volunteer and uses students to assist with the physical exams.
3. A group of medical students at UIC formed the Mobile Migrant Health Team, providing care to over 3,000 migrants since May. They visit police stations where migrants are sheltered, triaging patients, and prescribing over-the-counter medication overseen by licensed doctors. Any migrants presenting more severe health issues are sent to the nearest emergency room. Fundraising and a non-profit organization help fund any patient expenses. Separately, UIC doctors have also partnered with the National Youth Advocate Program to provide initial health exams for unaccompanied children seeking placement with foster families.
The US is currently home to around 85,000 children and adults from Africa, Asia, the Middle East and elsewhere who face health issues relating to undiagnosed illnesses and chronic conditions. Limited literacy rates, communication problems, lack of insurance and poverty contribute to these issues, which are difficult to handle for the conventional health system. However, doctors at a national network of clinics are ready to address these problems with cultural sensitivity and an understanding of the refugee patient experience.
The refugee and immigrant health clinic at the Cone Health Family Medicine Residency program in Greensboro, North Carolina is one of several such initiatives run by US medical schools and teaching hospitals. As the clinic director, Dr. Jeffrey Walden prepares medical students and residents to offer ongoing care to refugee and immigrant patients. Over 800 refugees from Sudan, Congo, Iraq and Syria are resettled each year in Guilford County, North Carolina, where the clinic is situated.
The clinic uses an interdisciplinary approach and care offered is often dependent on where the refugees come from. Most come with active cases of diseases like diabetes, hypertension and HIV that are yet to be diagnosed. Other health problems include latent tuberculosis, malaria, parasites and psychiatric illnesses. The health needs of the refugees often result in more time spent by doctors then envisioned by the insurance plans the refugees receive when they first arrive in the US. However, the insurance plans expire after several months, which affects the refugees’ access to healthcare.
Culturally sensitive interventions are also being implemented to improve refugee health. For instance, refugees visiting the Family Health Center of Worcester clinic in Massachusetts are offered assistance in navigating the US healthcare system by the same attending physician or global health fellow during every visit. They can also attend the clinic with their families to remove language and transportation barriers. The clinic has about 11 interpreters certified to attend patients speaking 43 languages.
Most clinics that offer such services often work with resettlement agencies that offer case managers and volunteers for refugees. They also perform health interventions beyond medical caregiving. For instance, the Nationalities Services Center (NSC) worked with local shops to increase their stock of B12-enriched foods to cater to the dietary needs of Bhutanese refugees at the Jefferson Center for Refugee Health run by Thomas Jefferson University’s Department of Family and Community Medicine. The model of the refugee health clinic run by the NSC was replicated across several universities.
As a result, the Philadelphia Refugee Health Collaborative which consists of 8 refugee health clinics and 3 resettlement agencies was formed in 2010. It provides a shared system of health and social care to refugees in need and offers resources and training in areas like cultural competency, health and resettlement to organizations working with refugees. It also seeks to put the competition between organizations aside to focus on creating a system suited for the refugees.
Sources:
 To solve for doctor shortages, states ease licensing for foreign-trained physicians : Shots – Health News
To solve for doctor shortages, states ease licensing for foreign-trained physicians : Shots – Health News Salud!
Salud! Trump deportation pledge raises concern over U.S. health system
Trump deportation pledge raises concern over U.S. health system Immigrants: Always Carry These Documents
Immigrants: Always Carry These Documents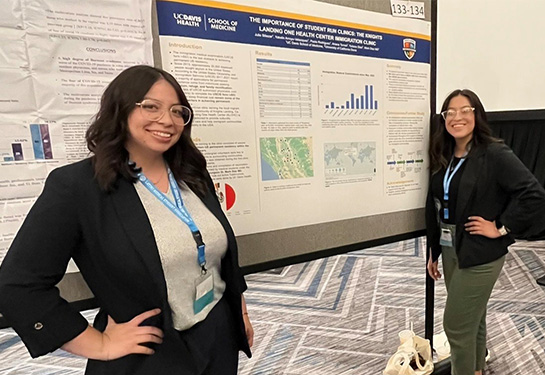 Medical students earn top honors at national conference
Medical students earn top honors at national conference Refugee Health Clinics Help New Arrivals, Provide Training Ground for Students and Residents
Refugee Health Clinics Help New Arrivals, Provide Training Ground for Students and Residents





Leave a Reply